Guide to Treating Foot Ulcers in Diabetes: Effective Solutions and Best Practices
Are you or a loved one living with diabetes? Foot ulcers can be a common and potentially serious complication of this chronic condition. In fact, studies show that up to 25% of all people with diabetes will develop a foot ulcer at some point. Treating foot ulcers in diabetes requires a comprehensive approach that addresses not only the wound itself but also the underlying causes and associated risks.
In this complete guide, we will explore the most effective solutions and best practices for treating foot ulcers in diabetes. From wound care techniques and dressings to offloading devices and footwear recommendations, we will leave no stone unturned in our quest to help you find the optimal treatment options for your foot ulcers.
We'll also delve into the importance of managing blood sugar levels, understanding the role of infection, and adopting healthy lifestyle habits to enhance the healing process. Whether you're a healthcare professional or someone personally affected by foot ulcers in diabetes, this guide is your one-stop resource for valuable information and actionable insights. Let's take a step towards better foot ulcer treatment together.
Understanding foot ulcers in diabetes
Foot ulcers are a common complication of diabetes, but what exactly are they? A foot ulcer is an open sore or wound that typically develops on the bottom of the foot. It is often a result of nerve damage (neuropathy) and reduced blood flow (peripheral arterial disease), both of which are common complications of diabetes. When neuropathy affects the feet, it can lead to loss of sensation, making it difficult to detect injuries or pressure points that can cause ulcers. Additionally, poor blood flow can impair the body's ability to heal wounds, further increasing the risk of foot ulcers.
Causes and risk factors of foot ulcers in diabetes
The development of foot ulcers in diabetes is influenced by various factors:
Neuropathy: Loss of protective sensation due to neuropathy can prevent individuals from feeling pain or discomfort, making them unaware of injuries or pressure points that lead to ulcers.
Poor Blood Flow: Peripheral arterial disease, characterized by reduced blood flow to the extremities, impedes the healing process and increases the risk of ulcers.
Foot Deformities: Structural abnormalities such as bunions or hammertoes can create areas of increased pressure, contributing to ulcer formation.
Calluses: Thickened areas of skin, often formed due to repetitive pressure or friction, can develop into ulcers if not properly managed.
Foot Trauma: Injuries such as cuts, burns, or blisters, especially when unnoticed due to neuropathy, can progress to ulcers.
High Blood Sugar Levels: Prolonged periods of elevated blood glucose levels impair wound healing and increase susceptibility to infections, exacerbating ulcer development.
Understanding these causes and risk factors is crucial for preventing foot ulcers in diabetes through proactive management and care.
Signs and symptoms of foot ulcers in diabetes
Identifying foot ulcers in diabetes requires vigilance. Here are signs and symptoms to watch for:
Painless Ulcers: Some ulcers may not cause pain, making regular foot inspections crucial for detection.
Redness, Inflammation, or Drainage: These are common signs of ulceration and should prompt immediate attention.
Changes in Skin: Look for areas of increased warmth, swelling, or skin discoloration, which may indicate underlying issues.
Foul Odors or Discharge: These can signal infection and require prompt medical evaluation.
Regular foot inspections, especially for individuals with diabetes, help catch ulcers early, enhancing treatment outcomes and preventing complications.
Importance of early detection and treatment
Treating foot ulcers in diabetes requires prompt action. The earlier an ulcer is detected, the better the chances of successful healing and prevention of complications. Delayed or inadequate treatment can lead to infection, which can spread to the bone or surrounding tissues, potentially resulting in the need for amputation. Therefore, if you notice any signs or symptoms of a foot ulcer, it is crucial to seek medical attention immediately. Early intervention can significantly improve outcomes and reduce the risk of severe complications.
Effective solutions for treating foot ulcers in diabetes
Treating foot ulcers in diabetes requires a comprehensive approach. Here are effective solutions:
Wound Cleaning and Dressing: Cleanse the wound gently with mild soap and water, then apply appropriate dressings like hydrocolloids, foams, or alginates to create a moist environment conducive to healing and infection prevention.
Offloading: Reduce pressure on the ulcer by offloading the affected foot. Specialized footwear like custom-made shoes or therapeutic sandals distributes weight evenly, aiding in optimal blood flow and tissue regeneration.
Offloading Devices: In some cases, additional offloading devices such as removable cast boots or specialized braces may be recommended to provide extra support and protection to the ulcer site.
Multidisciplinary Care: Involve healthcare professionals such as podiatrists, wound care specialists, and diabetes educators for tailored treatment plans and ongoing monitoring.
By combining these approaches, individuals can effectively manage foot ulcers in diabetes, promoting healing and preventing complications.
Best practices for foot ulcer care and prevention
Prevention plays a crucial role in managing foot ulcers, especially for individuals with diabetes. Here are some best practices for foot ulcer care and prevention:
Regular Foot Inspections: Check your feet daily for any changes, cuts, blisters, or signs of infection. Early detection allows for prompt treatment and prevents complications.
Maintain Foot Hygiene: Keep your feet clean and dry to prevent skin breakdown. Avoid soaking your feet for prolonged periods, as it can lead to maceration of the skin.
Moisturize Properly: Moisturize your feet regularly, but avoid applying lotion between the toes, as it can create a moist environment conducive to fungal infections.
Temperature Awareness: Avoid exposing your feet to extreme temperatures, as it can cause skin damage. Always wear appropriate footwear in hot or cold weather.
Choose Proper Footwear: Opt for shoes that fit well, provide adequate support, and have a wide toe box to reduce pressure and friction. Avoid tight shoes or high heels, as they can cause irritation and skin breakdown.
Consider Custom-made Shoes: Individuals at high risk of foot ulcers may benefit from custom-made shoes or orthotics, which ensure a proper fit and minimize the risk of injury.
Avoid Walking Barefoot: Always wear shoes or protective footwear, even indoors, to prevent injuries from sharp objects or uneven surfaces.
Regular Foot Care by Professionals: Schedule regular foot exams with a healthcare provider, podiatrist, or diabetes care team. They can assess your foot health, provide education on foot care practices, and address any concerns promptly.
By following these best practices for foot ulcer care and prevention, individuals with diabetes can significantly reduce the risk of developing new ulcers and maintain overall foot health.
Medical interventions for severe foot ulcers
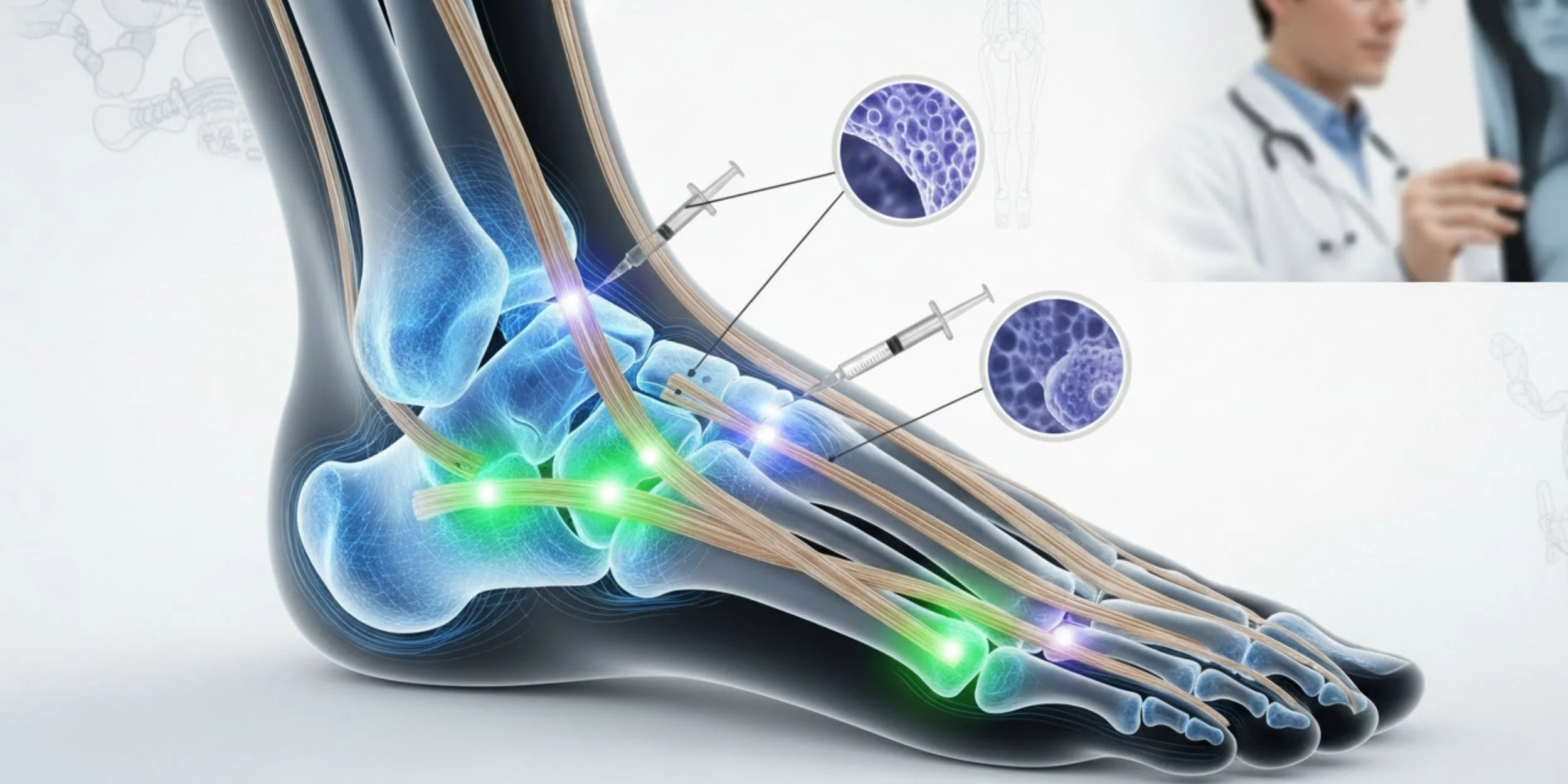
Severe foot ulcers, especially in diabetes patients, demand prompt and targeted medical interventions to prevent complications. Here's a concise overview:
Wound Debridement: Removing dead tissue to foster healing.
Topical Therapies: Using antimicrobial agents and advanced dressings.
Offloading: Relieving pressure on ulcers with specialized footwear.
Vascular Interventions: Restoring blood flow to aid healing.
Hyperbaric Oxygen Therapy: Enhancing tissue oxygenation for healing.
Biological Therapies: Stimulating tissue regeneration.
Surgical Options: Skin grafting or flap reconstruction when needed.
Multidisciplinary Care Teams: Collaborative approach for tailored care.
Comprehensive management, involving these interventions and close monitoring, is essential for optimizing outcomes and preventing complications in severe foot ulcers.
Diabetic footwear and orthotics for foot ulcer prevention
Diabetic footwear and orthotics are instrumental in preventing foot ulcers among individuals with diabetes. Here's why:
Specialized Design: Diabetic shoes feature extra depth, cushioning, and a wide toe box, which alleviate pressure points and offer superior support, reducing the risk of ulcers.
Orthotics for Weight Distribution: Custom-made insoles or arch supports distribute weight evenly across the foot, minimizing the likelihood of developing ulcers due to uneven pressure.
Consultation with Healthcare Professionals: Seek guidance from podiatrists or orthotists to ensure the footwear or orthotics meet your specific needs. Their expertise ensures proper fitting and personalized recommendations.
Individualized Assessments: Healthcare professionals assess your foot health and tailor recommendations accordingly, addressing unique concerns and risk factors.
Regular Follow-up: Continuous monitoring and adjustments are essential to maintain the effectiveness of diabetic footwear and orthotics, ensuring ongoing protection against ulcers.
By incorporating diabetic footwear and orthotics into your foot care routine under professional guidance, you can significantly lower the risk of foot ulcers and safeguard your foot health in diabetes management.
Lifestyle changes for managing foot ulcers and diabetes
Managing foot ulcers in diabetes requires holistic lifestyle changes beyond medical treatments. Here's how:
Blood Sugar Control: Monitor levels regularly, follow a balanced diet, and adhere to medication or insulin regimens to optimize healing and reduce infection risks.
Weight Management: Maintain a healthy weight to alleviate pressure on feet and improve overall health, aiding in wound healing.
Regular Exercise: Engage in low-impact activities to enhance blood circulation, vital for healing. Proper footwear minimizes injury risks during exercise.
Quit Smoking: Smoking hampers blood flow, hindering healing processes. Quitting smoking accelerates recovery and reduces ulcer recurrence risks.
By embracing these lifestyle changes alongside medical treatments, individuals can effectively manage foot ulcers in diabetes, promoting healing and preventing future complications.
Conclusion: Taking control of foot ulcers in diabetes
Foot ulcers in diabetes can be a challenging and potentially serious complication, but with the right knowledge and proactive approach, they can be effectively treated and prevented. By understanding the causes and risk factors, recognizing the signs and symptoms, and implementing the most effective solutions and best practices, individuals with diabetes can take control of their foot ulcer management. Remember, early detection, prompt treatment, and adopting healthy lifestyle habits are key to enhancing healing, preventing complications, and maintaining overall foot health. Let's continue taking strides towards better foot ulcer treatment together.