The Silent Threat: Understanding Diabetic Foot Infections
In the labyrinth of diabetic complications, foot infections emerge as a silent yet formidable threat, often overshadowed by more widely discussed issues like cardiovascular disease and retinopathy. However, for the millions living with diabetes worldwide, the risk of developing a foot infection is not just a footnote in their health journey—it's a critical concern that demands attention, understanding, and proactive care.
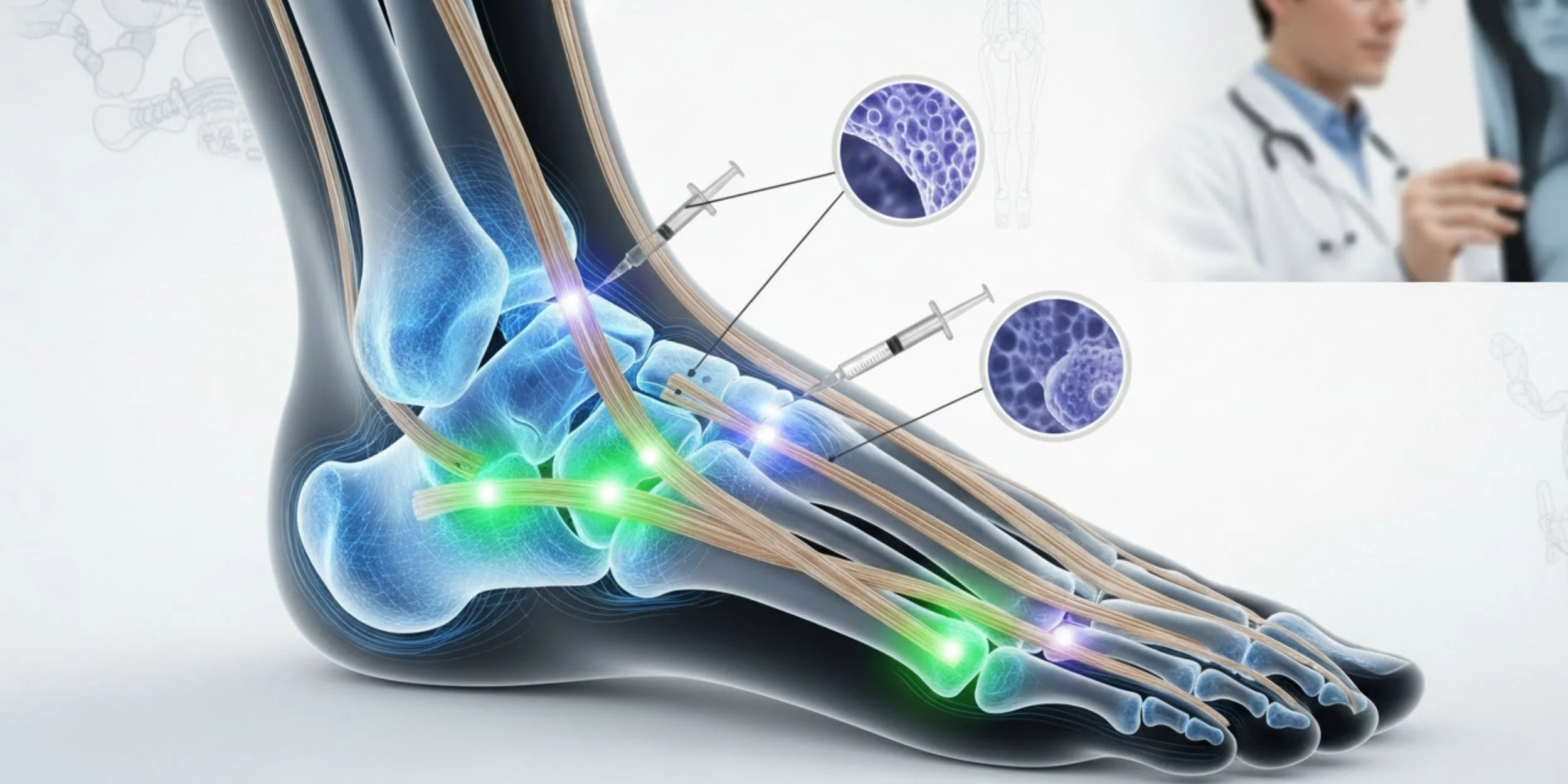
Diabetic foot infections represent a complex interplay between the systemic effects of diabetes and the vulnerability of the feet to injury and infection. As glucose levels fluctuate and remain elevated over time, the intricate network of blood vessels and nerves in the feet can become compromised, setting the stage for a cascade of problems that, if left unchecked, can lead to severe consequences, including amputation.
This comprehensive guide aims to shed light on the often-overlooked realm of diabetic foot infections, offering insights into their types, early warning signs, potential complications, and the crucial role that podiatrists play in both prevention and treatment. By understanding the nuances of this condition, individuals with diabetes and their caregivers can be better equipped to recognize early signs, seek timely intervention, and implement effective prevention strategies.
Types of Diabetic Foot Infections
Diabetic foot infections are not a monolithic entity but rather a spectrum of conditions that can affect different structures within the foot. Understanding these distinctions is crucial for proper diagnosis and treatment:
1. Cellulitis
Cellulitis is perhaps the most common type of diabetic foot infection, characterized by inflammation of the skin and underlying soft tissues. It typically begins as a localized area of redness, warmth, and swelling, often triggered by a small cut or abrasion that serves as an entry point for bacteria. In individuals with diabetes, the reduced sensation in the feet (neuropathy) can mask the initial injury, allowing the infection to progress unnoticed.
The danger of cellulitis lies in its potential to spread rapidly, especially in the context of compromised circulation common in diabetes. What starts as a small, seemingly innocuous patch can quickly evolve into a life-threatening condition if not addressed promptly.
2. Osteomyelitis
When infections penetrate deeper into the foot, they can reach the bone, leading to osteomyelitis. This severe condition is particularly insidious in diabetic patients, as the reduced blood flow to the extremities can hamper the body's natural defense mechanisms and the delivery of antibiotics to the affected area.
Osteomyelitis often develops as a complication of untreated soft tissue infections or chronic wounds. The diagnosis can be challenging, often requiring advanced imaging techniques like MRI or bone scans, as well as bone biopsies in some cases. Treatment typically involves long-term antibiotic therapy and, in severe cases, surgical intervention to remove infected bone tissue.
3. Necrotizing Fasciitis
While rare, necrotizing fasciitis represents one of the most severe and rapidly progressing forms of diabetic foot infections. This "flesh-eating" bacterial infection spreads along the fascia, the connective tissue that surrounds muscles, blood vessels, and nerves. The compromised immune response and reduced sensation associated with diabetes can allow this aggressive infection to advance undetected until it reaches a critical stage.
Necrotizing fasciitis is a medical emergency requiring immediate surgical intervention and intensive antibiotic therapy. The mortality rate for this condition remains high, underscoring the importance of early recognition and prompt treatment.
4. Diabetic Foot Ulcers
While not an infection per se, diabetic foot ulcers deserve mention as they often serve as a precursor to infections. These open sores or wounds, typically occurring on the bottom of the foot, result from a combination of factors including neuropathy, poor circulation, and mechanical stress on the foot.
Left untreated, these ulcers can deepen, extending to tendons, bones, and other deeper structures. They also provide an ideal environment for bacterial growth, significantly increasing the risk of infection. Managing diabetic foot ulcers requires a multidisciplinary approach, involving wound care specialists, podiatrists, and vascular surgeons to address the underlying causes and promote healing.
Early Warning Signs
The key to preventing serious complications from diabetic foot infections lies in early detection. However, the very nature of diabetes—particularly the neuropathy that often accompanies it—can mask traditional warning signs. This makes it imperative for individuals with diabetes and their caregivers to be vigilant and proactive in monitoring foot health.
Here are some critical early warning signs to watch for:
1. Skin Changes
Any alterations in the appearance of the skin on the feet should be taken seriously. This includes:
Redness or discoloration, especially if it spreads or intensifies over time
Warmth in a localized area, which may indicate inflammation
Swelling or puffiness, particularly if it's asymmetrical (affecting one foot more than the other)
Changes in skin texture, such as areas that become unusually dry, scaly, or shiny
It's important to note that these changes may be subtle at first and might not be accompanied by pain due to neuropathy. Regular visual inspection of the feet, including the soles and between the toes, is crucial.
2. Wounds or Breaks in the Skin
Any breach in the skin's integrity can serve as an entry point for bacteria. This includes:
Cuts or scrapes, no matter how small
Blisters or calluses that have broken open
Cracks in the skin, especially on the heels
Ingrown toenails that pierce the surrounding skin
In individuals with diabetes, even minor wounds can be slow to heal and prone to infection. Any wound that doesn't show signs of improvement within a few days warrants professional attention.
3. Unusual Sensations
While neuropathy can dull sensation, some individuals may experience new or changing sensations as an early sign of infection:
Tingling or burning sensations
Increased sensitivity or pain in an area that was previously numb
A feeling of fullness or pressure in the foot
These sensations, particularly if they're new or localized to a specific area, should not be ignored.
4. Changes in Foot Temperature
Using a infrared thermometer to measure foot temperature can be an effective early detection method. A difference of more than 2.2°C (4°F) between corresponding points on each foot may indicate inflammation or infection in the warmer foot.
5. Drainage or Odor
Any unusual discharge from a wound or between the toes, especially if accompanied by an unpleasant odor, is a red flag for infection. This can range from clear fluid to pus and may be accompanied by a foul smell.
6. Systemic Symptoms
In some cases, early signs of a foot infection may manifest as systemic symptoms:
Unexplained fever or chills
Fatigue or malaise
Elevated blood glucose levels that are difficult to control
These symptoms, especially when combined with any local foot changes, warrant immediate medical attention.
Complications
The consequences of untreated or poorly managed diabetic foot infections can be severe and far-reaching, extending well beyond the foot itself. Understanding these potential complications underscores the critical importance of early detection and aggressive treatment:
1. Amputation
Perhaps the most feared complication, amputation remains a significant risk for individuals with advanced diabetic foot infections. The progression from a seemingly minor infection to a life-altering amputation can be alarmingly swift, particularly in cases where circulation is severely compromised or infection has spread to the bone.
Statistics paint a sobering picture: people with diabetes face a risk of lower extremity amputation that is 15 to 40 times higher than that of the general population. Moreover, studies have shown that up to 85% of diabetes-related amputations are preceded by a foot ulcer, highlighting the crucial importance of ulcer prevention and early intervention.
The impact of amputation extends far beyond the physical loss of a limb. It can profoundly affect mobility, independence, and quality of life. Additionally, individuals who undergo a lower extremity amputation face a significantly higher risk of mortality in the years following the procedure, with some studies suggesting a five-year mortality rate as high as 50%.
2. Systemic Infection
What begins as a localized foot infection can, if left unchecked, evolve into a systemic infection that affects the entire body. Bacteria from the foot can enter the bloodstream, leading to septicemia, a life-threatening condition characterized by widespread inflammation and organ dysfunction.
The risk of systemic infection is particularly high in individuals with diabetes due to their compromised immune function. Symptoms of systemic infection include high fever, rapid heart rate, confusion, and in severe cases, septic shock. This condition requires immediate hospitalization and intensive treatment, often including intravenous antibiotics and supportive care.
3. Chronic Wound Development
Diabetic foot infections can lead to the development of chronic, non-healing wounds. These wounds, often in the form of ulcers, can persist for months or even years, significantly impacting quality of life and increasing the risk of recurrent infections.
Chronic wounds are notoriously difficult to treat, often requiring specialized wound care, offloading devices to reduce pressure on the affected area, and in some cases, advanced therapies such as negative pressure wound therapy or bioengineered skin substitutes. The persistence of these wounds not only increases the risk of infection but also contributes to social isolation, depression, and reduced mobility.
4. Charcot Foot
While not a direct complication of infection, Charcot foot is a severe deformity that can develop in individuals with diabetic neuropathy. The loss of sensation can lead to repeated trauma and inflammation, causing the bones in the foot to weaken and eventually fracture and dislocate.
The presence of an infection can exacerbate the Charcot process, accelerating bone destruction and deformity. Once established, Charcot foot significantly increases the risk of ulceration and subsequent infection, creating a vicious cycle of complications.
5. Psychosocial Impact
The complications of diabetic foot infections extend beyond physical health, profoundly affecting mental and emotional well-being. Chronic wounds, repeated hospitalizations, and the constant threat of amputation can lead to:
Depression and anxiety
Social isolation
Loss of employment and financial strain
Reduced quality of life
These psychosocial impacts are often under recognized but play a crucial role in overall health outcomes and treatment adherence.
Role of Podiatrists
In the complex landscape of diabetic foot care, podiatrists emerge as pivotal figures, blending specialized knowledge with a holistic approach to patient care. Their role extends far beyond treating existing infections; they are at the forefront of prevention, early detection, and comprehensive management of diabetic foot complications.
Preventive Care
Podiatrists play a crucial role in preventing diabetic foot infections through several key strategies:
Regular Foot Examinations: Routine podiatric check-ups allow for the early identification of potential problems. During these examinations, podiatrists assess circulation, nerve function, and structural integrity of the feet. They can detect subtle changes that might escape the notice of patients or general practitioners.
Patient Education: Podiatrists serve as educators, empowering patients with the knowledge and skills needed for effective self-care. This includes teaching proper foot hygiene, nail care techniques, and the importance of daily foot inspections. They also provide guidance on appropriate footwear and the use of orthotics to reduce pressure points and prevent ulceration.
Risk Assessment: By evaluating factors such as neuropathy, vascular health, and foot biomechanics, podiatrists can stratify patients according to their risk of developing foot complications. This allows for the implementation of tailored preventive strategies and determines the frequency of follow-up visits.
Biomechanical Corrections: Addressing structural foot problems through orthotics, specialized footwear, or in some cases, corrective surgery can significantly reduce the risk of ulceration and subsequent infection.
Early Detection and Intervention
The specialized training of podiatrists makes them uniquely qualified to detect early signs of foot problems in diabetic patients:
Advanced Diagnostic Techniques: Podiatrists utilize a range of diagnostic tools, including doppler ultrasound for vascular assessment, monofilament testing for neuropathy, and thermography for detecting inflammation. These techniques can identify problems before they become clinically apparent.
Prompt Treatment of Minor Issues: What might seem like a minor problem—a small cut, a callus, or an ingrown toenail—can quickly escalate in a diabetic foot. Podiatrists can address these issues promptly, preventing them from developing into more serious complications.
Wound Care Expertise: For patients who develop ulcers, podiatrists are skilled in advanced wound care techniques. This includes debridement (removal of dead tissue), application of appropriate dressings, and the use of offloading devices to promote healing.
Comprehensive Management of Infections
When infections do occur, podiatrists are central to the management process:
Accurate Diagnosis: Through clinical examination and, when necessary, imaging studies or laboratory tests, podiatrists can determine the extent and severity of an infection.
Targeted Treatment: This may include prescribing appropriate antibiotics, performing surgical drainage or debridement, and implementing advanced wound care protocols.
Multidisciplinary Coordination: Podiatrists often serve as the coordinators of care, collaborating with other specialists such as endocrinologists, vascular surgeons, and infectious disease experts to ensure comprehensive treatment.
Long-term Follow-up: After the acute phase of an infection, podiatrists continue to monitor patients, addressing any residual issues and implementing strategies to prevent recurrence.
Limb Salvage
In cases of severe infection or advanced complications, podiatrists play a crucial role in limb salvage efforts:
Surgical Interventions: This may include procedures to remove infected tissue, restore blood flow, or correct deformities that contribute to ulceration.
Alternative Treatments: Podiatrists may employ advanced therapies such as hyperbaric oxygen treatment or bioengineered tissue grafts to promote healing in challenging cases.
Rehabilitation Planning: Working closely with physical therapists and orthotists, podiatrists help patients regain mobility and function after recovering from severe infections or surgical interventions.
Conclusion
Diabetic foot infections are preventable and manageable with early detection and proactive care. Regular foot inspections, timely medical attention, and collaboration with podiatrists can significantly reduce the risk of severe complications. Take charge of your foot health and consult a podiatrist to avoid preventable issues and maintain a good quality of life.